Tinnitus and Stress – Breaking the Anxiety Cycle
.avif)
Breaking the Anxiety Cycle: How Stress and Tinnitus Fuel Each Other (and What Helps)
Tinnitus can be loud. But what often makes it feel unbearable is the loop around it: stress increases the ringing, the ringing increases stress, and your brain gets stuck on high alert.
This article explains the bidirectional relationship between tinnitus and anxiety/stress and gives evidence-based, practical strategies to interrupt the feedback loop—without overpromising a cure.
code Code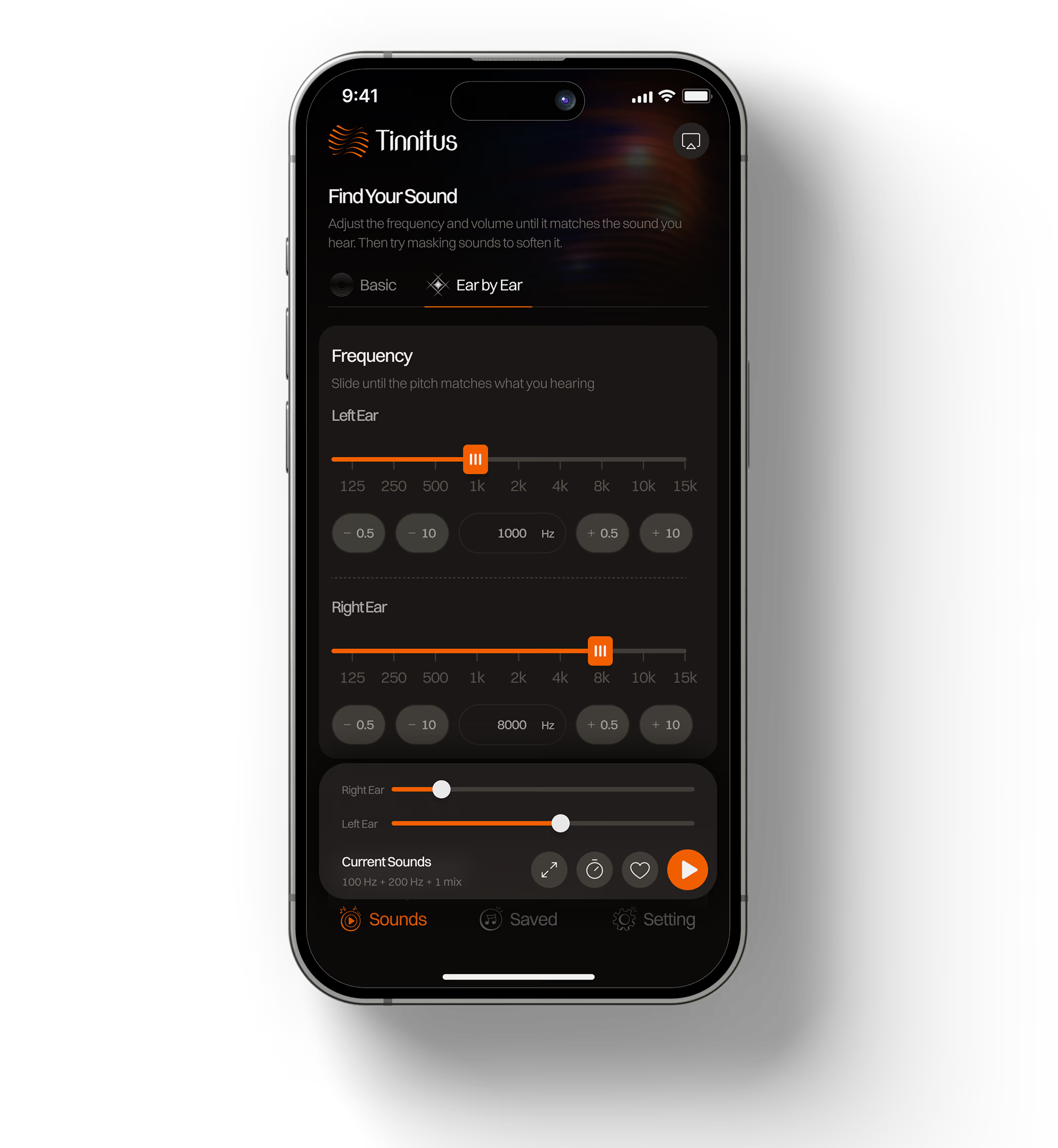
Why tinnitus and anxiety feel inseparable
The tinnitus–stress loop (what’s happening)
Think of tinnitus as a signal your brain notices. Stress changes how your brain filters signals.
- Stress/anxiety increases tinnitus perception: Your nervous system shifts into “threat scanning.” Attention narrows, silence feels unsafe, and the tinnitus signal becomes “important.”
- Tinnitus increases stress/anxiety: The sound can feel unpredictable and uncontrollable. That uncertainty triggers worry (“What if it gets worse?”), which increases arousal.
- Arousal makes the brain listen harder: More monitoring → stronger perception → more stress.
This is why two people can have similar tinnitus loudness but very different tinnitus distress. Clinical resources consistently recommend psychological approaches (especially CBT) for tinnitus distress, alongside education and coping tools like sound therapy (nhs.uk).
Why tinnitus gets worse when you’re stressed (and at night)
- 1) Your brain increases “gain”: When the brain expects danger, it turns up sensitivity to signals. Tinnitus stands out more.
- 2) Silence increases contrast: At night, background sound drops. The tinnitus becomes the “loudest thing in the room,” so your brain locks onto it.
- 3) Sleep loss amplifies everything: Poor sleep increases irritability, reduces coping capacity, and raises baseline arousal—making tinnitus harder to ignore.
What “evidence-based relief” actually means for tinnitus
There is no single universal cure, but there are approaches with evidence for reducing impact:
CBT (Cognitive Behavioral Therapy) reduces tinnitus distress: Guidelines and reviews support CBT for persistent, bothersome tinnitus, primarily by reducing distress and improving coping rather than “erasing the sound” (guidelinecentral.com).
Sound therapy can help by reducing contrast and supporting habituation: Sound therapy may help by masking tinnitus, distracting, or helping you habituate over time—your brain treats the sound as unimportant (nidcd.nih.gov).
A) Reduce arousal
Try to bring your threat level down from 8/10 to 5/10 through nervous system regulation.
B) Stop monitoring
Attention training helps reduce the "checks" your brain makes to see if the sound is still there.
C) Reduce silence
Use consistent low-level sound to make tinnitus less dominant in your environment.
Practical strategies that work in real life
1) The 60-second reset (for spikes)
- Step 1 (10s): Label it. “This is tinnitus + stress. My brain is on alert.”
- Step 2 (30s): Slow exhale breathing. Inhale normally, exhale longer than inhale (e.g., 4 in / 8 out).
- Step 3 (20s): Add gentle sound. Low-level noise or a neutral soundscape.
2) Stop the “tinnitus checking” habit
When you notice yourself scanning for the sound, switch attention to one external anchor for 20 seconds: feel your feet on the floor, listen for 3 external sounds, or name 5 objects you can see.
3) Choose the right noise

White Noise
(High Rings)
.webp)
Pink Noise
(Soft/Balanced)
.webp)
Brown Noise
(Deep/Sleep)

Green Noise
(Nature/Calm)
Want fast relief tools—without a program?
Match your tinnitus tone, choose a masking sound, and save custom mixes for sleep and focus.
Download Tinnitus Relief AppPrefer to learn first?
Start with our comprehensive guides to build your management plan: